Burnout has become the default explanation for healthcare worker distress since COVID-19.
Exhausted? Burnout.
Dreading your shift? Burnout.
Can't sleep because you're replaying your day? Burnout.
The proposed solution? Resilience. Find your why. Practice self-care. Meditate between patients.
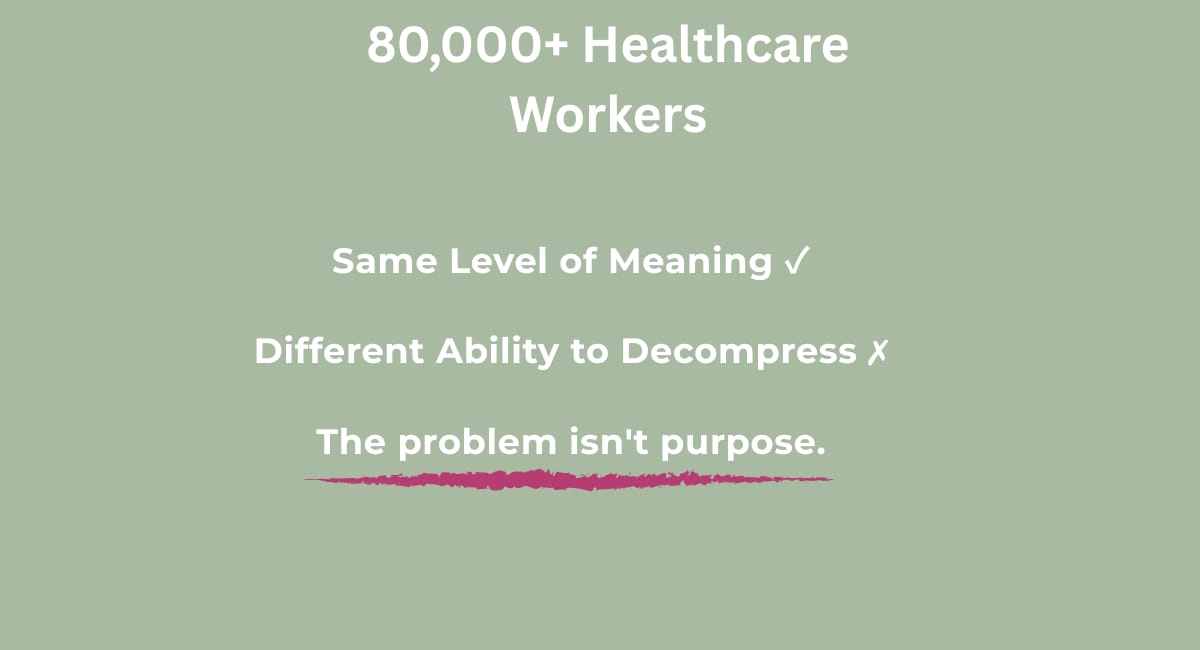
But a Harvard Business Review study of more than 80,000 healthcare workers suggests we've been focused on the wrong variable.
The Study: Activation vs. Decompression
Researchers measured two characteristics associated with burnout resilience:
Activation: The extent to which someone is motivated by their work and finds it meaningful.
Decompression: The degree to which someone can withdraw, recharge, and enjoy life outside of work.
They measured decompression with questions like:
I rarely lose sleep over work issues
I am able to free my mind from work when away from it
I can enjoy personal time without focusing on work matters
I am able to disconnect from work communications during free time
What They Found
Every group physicians, nurses, and non-clinical staff scored the same on activation. Everyone found meaning in their work.
But they differed significantly on decompression. Physicians scored lowest.
The critical finding: For clinicians, the ability to decompress was more strongly correlated with job satisfaction than finding meaning in work.
Translation: Helping healthcare workers "find their why" isn't the bottleneck. The bottleneck is that we can't mentally clock out.
Why Wellness Programs Miss This
Healthcare workers already have meaning. We know why we do this work. We care deeply about our patients.
The problem isn't activation. It's decompression.
And decompression isn't something you can achieve by pausing between appointments or taking deep breaths.
Because decompression isn't a time management problem. It's a neurological problem.
What the Questions Actually Reveal
Look at what the decompression questions are really asking:
"I rarely lose sleep over work issues." → Work thoughts are keeping you awake.
"I am able to free my mind from work when away from it." → You're home, but mentally still at the bedside.
"I can enjoy personal time without focusing on work matters." → You're with family, but mentally triaging patients.
This is mental spillover.
Your brain continues working after your shift ends because it's processing incomplete cognitive loops:
Did I chart that drain output?
Should I have called the provider sooner?
Is my patient okay right now?
These tasks have no clean endpoint. So your brain keeps processing—seeking closure, replaying scenarios, problem-solving.
You're not "choosing" to think about work. Your brain is doing what it's designed to do: attempt to close unfinished loops.
Why Current Solutions Don't Work
Most interventions focus on:
Time management → Leave on time, take your breaks
Resilience building → Develop coping skills, increase stamina
Meaning-making → Remember your why, reconnect with purpose
But none of these address the neurological mechanism keeping your brain in work mode.
You can leave exactly on time and still spend three hours mentally reviewing your shift.
Resilience training builds stamina to withstand stress, but doesn't give your brain permission to stop processing work tasks.
And the study already showed meaning isn't where clinicians are struggling.
The Real Question
If decompression is the critical factor for clinician well-being, and mental spillover prevents decompression, then the question isn't:
"How do we help healthcare workers find meaning?"
The question is:
"What gives the brain neurological permission to close work loops and actually log out?"
That's not a resilience question. It's an energy boundary question.
What This Means
The HBR study confirmed what I've observed across 10+ years in healthcare:
Experienced clinicians don't lack meaning. They lack the ability to mentally clock out.
The burnout discourse has focused on activation reconnecting with purpose, building resilience.
But the data suggests we should focus on decompression understanding why the clinical brain won't shut off.
This isn't about working less or caring less.
It's about understanding the specific mechanism mental spillover that keeps us mentally tethered to work.
And building energy boundaries that actually interrupt the pattern.
More on that soon.
Source:
Mylod, D.E., & Lee, T.H. (2018). Helping Health Care Workers Avoid Burnout. Harvard Business Review. Retrieved from https://hbr.org/2018/10/helping-health-care-workers-avoid-burnout
What's next?
This study confirmed what I've been observing: clinicians don't lack meaning they lack the ability to mentally clock out.
Over the next few weeks, I'll be breaking down:
The Mental Spillover Cycle (why your brain won't shut off)
What conventional solutions miss
The Permission Protocol (what actually interrupts the pattern)
Want these insights delivered weekly?